Mental health is a critical aspect of our overall physical, emotional, and psychological wellbeing. Unfortunately, many people struggle with mental health issues at some point in their lives, and accessing the proper therapy can be expensive. The good news is that Medicare may provide coverage for mental health therapy, so understanding what is covered can help those in need get the help they need. In this article, we will explore the question, “Does Medicare cover mental health therapy?”
Yes, Medicare covers mental health therapy like individual psychotherapy, family therapy, and group psychotherapy. Medicare Part B covers your visits to a psychiatrist, clinical psychologist, or other qualified healthcare provider. You will pay 20% of the Medicare-approved amount for the doctor’s services, and the Part B deductible applies. You may also need to pay a coinsurance amount for mental health services you receive from a hospital outpatient clinic or community mental health center.
Contents
- Does Medicare Cover Mental Health Therapy?
- What Services Does Medicare Cover for Mental Health Therapy?
- What Is Not Covered by Medicare for Mental Health Therapy?
- What Is the Cost for Mental Health Therapy Services Covered by Medicare?
- Does Medicare Cover Mental Health Therapy in a Skilled Nursing Facility?
- Does Medicare Cover Mental Health Therapy in an Assisted Living Facility?
- What Are the Eligibility Requirements for Mental Health Therapy Services Covered by Medicare?
- How Do I Find a Medicare-Approved Mental Health Therapy Provider?
- Few Frequently Asked Questions
- 1. What is mental health therapy?
- 2. Does Medicare cover mental health therapy?
- 3. How do I access Medicare rebates for mental health therapy?
- 4. Who is eligible for Medicare rebates for mental health therapy?
- 5. Are there any limits on the number of sessions of mental health therapy that are covered by Medicare?
- 6. What other costs are associated with mental health therapy?
- Medicare Behavioral Health Coverage
Does Medicare Cover Mental Health Therapy?
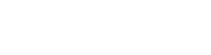
Mental health therapy is an important part of overall health and well-being. Medicare, the federal health insurance program for people 65 and older, covers mental health therapy in many cases. Medicare Part B covers outpatient mental health services, such as individual and group therapy, and Part A covers inpatient mental health services in a hospital.
Medicare Part B covers mental health therapy services, such as individual and group therapy, provided you have a doctor’s prescription and the therapy is considered medically necessary. Part B also covers psychiatric diagnostic exams and psychological and neuropsychological tests. Medicare Part A covers inpatient mental health care in a hospital, and Part D covers certain prescription drugs used to treat mental health issues.
What Services Does Medicare Cover for Mental Health Therapy?
Medicare Part B covers outpatient mental health therapy services, such as individual and group therapy, provided you have a doctor’s prescription and the therapy is considered medically necessary. Medicare Part B also covers psychiatric diagnostic exams and psychological and neuropsychological tests.
Inpatient mental health services are covered by Medicare Part A. Part A covers mental health care in a hospital if you are admitted as an inpatient. Inpatient mental health care includes meals, tests, and medications while you are in the hospital.
What Is Not Covered by Medicare for Mental Health Therapy?
Medicare Part B does not cover most long-term mental health therapy services, such as psychotherapy, family therapy, or marriage counseling, unless they are medically necessary. Medicare Part D does not cover most psychotherapeutic drugs, such as antidepressants and antipsychotic medications.
Mental health therapy services provided in a doctor’s office are not covered by Medicare if the doctor does not accept assignment. Assignment means that the doctor agrees to accept the Medicare approved amount as payment in full for the service.
What Is the Cost for Mental Health Therapy Services Covered by Medicare?
Your share of the cost for mental health therapy services covered by Medicare Part B depends on the type of service you receive. Most mental health services are subject to the Part B deductible and coinsurance. The Part B deductible is the amount you must pay for Medicare-covered services before Medicare begins to pay its share. The Part B coinsurance is the amount you must pay after you meet your Part B deductible.
Does Medicare Cover Mental Health Therapy in a Skilled Nursing Facility?
Mental health therapy services provided in a skilled nursing facility are covered by Medicare Part A. Part A covers mental health care in a skilled nursing facility if you are admitted as an inpatient. Skilled nursing facility services include physical therapy, occupational therapy, speech therapy, and mental health therapy services.
Does Medicare Cover Mental Health Therapy in an Assisted Living Facility?
Mental health therapy services provided in an assisted living facility are not covered by Medicare. Medicare does not cover services provided in assisted living facilities, such as room and board, meals, housekeeping, and personal care services.
What Are the Eligibility Requirements for Mental Health Therapy Services Covered by Medicare?
To be eligible for mental health therapy services covered by Medicare, you must be enrolled in Medicare Part A and Part B, and the services must be deemed medically necessary. Medicare Part B covers mental health therapy services provided by a doctor or other health care provider who accepts assignment from Medicare.
How Do I Find a Medicare-Approved Mental Health Therapy Provider?
To find a Medicare-approved mental health therapy provider, you can search the Medicare Physician Compare website. The website provides detailed information about providers, including their qualifications, specialties, and accepted Medicare plans. You can also contact your local Medicare office for more information.
Few Frequently Asked Questions
1. What is mental health therapy?
Mental health therapy is a type of treatment used to help people manage and cope with mental health issues. It can include talking therapies such as cognitive behavioural therapy (CBT) and psychotherapy, and also other treatments such as art therapy, music therapy, and exercise. Mental health therapy can help people to understand their thoughts and feelings, and how to better manage them.
2. Does Medicare cover mental health therapy?
Yes, Medicare covers mental health therapy, as long as it is provided by a registered mental health professional. Medicare provides rebates for up to 10 individual and 10 group sessions of mental health therapy each year.
3. How do I access Medicare rebates for mental health therapy?
In order to access Medicare rebates for mental health therapy, you will need to visit your doctor and obtain a mental health treatment plan. The plan will need to be approved by Medicare before you can access the rebates.
4. Who is eligible for Medicare rebates for mental health therapy?
Anyone who is eligible for Medicare, and is referred to a registered mental health professional by their doctor, is eligible for Medicare rebates for mental health therapy.
5. Are there any limits on the number of sessions of mental health therapy that are covered by Medicare?
Yes, the number of sessions of mental health therapy that are covered by Medicare is limited to 10 individual and 10 group sessions each year.
6. What other costs are associated with mental health therapy?
In addition to the Medicare rebates, there may be other costs associated with mental health therapy, such as consultation fees. You may also need to pay for any additional services such as medications or tests. It is important to check with your mental health professional before you start therapy to find out what additional costs may be involved.
Medicare Behavioral Health Coverage
The answer to the question of whether or not Medicare covers mental health therapy is yes. Medicare coverage of mental health therapy is a crucial part of supporting the mental health of seniors, and it can provide the help that many people need to manage their mental health. However, it is important to keep in mind that Medicare coverage is limited, and it is best to check with your provider to make sure that the mental health services you need are covered. With the help of Medicare coverage, seniors can get the mental health services that they need to lead a healthy and fulfilling life.